Before the Diagnosis – How to Take Control of Your Health Before It’s Too Late
We’re living in the most medically advanced era in human history. From gene editing and AI diagnostics to personalized medicine and telehealth, science has given us tools that our ancestors could only dream of. Despite all this progress, we’re not getting healthier. In fact, chronic illness is rising at an alarming rate.

Heart disease, diabetes, cancer, autoimmune disorders, and neurodegenerative conditions are no longer confined to the elderly. They’re showing up in younger populations, and in many cases, they’re developing silently over years before diagnosis. If medical innovation is accelerating, why are so many of us still getting sicker?
One possible answer lies in the timing of our interventions.
In Eastern medicine, illness is seen as a progressive process. The traditional model includes six stages of disease pathogenesis, beginning with subtle imbalances long before symptoms emerge. Western medicine recognizes disease only at the 5th stage, when symptoms are undeniable and a medical diagnosis can be made. At this stage, the damage is already done and reversal is hard or impossible. The opportunity for prevention is missed.
This isn’t about blaming doctors or criticizing the healthcare system. Medical professionals are working under intense pressure, and the system simply isn’t built to offer a personalized, preventive approach to every individual. Sadly, the structure of modern healthcare is optimized to treat disease, not to prevent it.
Which means one critical truth remains: Your health is in your hands.

Source: Pixabay
There’s a saying from Eastern philosophy: “Saving the drowning is the business of the one who drowns.” It’s a stark but empowering reminder that while medicine can intervene, only you can take responsibility for your health before it’s too late.
That’s what this article is about – how to take control of your well-being before the diagnosis comes. Before the symptoms appear. Before your body sounds the alarm in ways that can’t be ignored.
Are you ready to stop waiting for illness, and start living with intention?
The Flawed Healthcare System: Treating Symptoms, Not Causes
Walk into any doctor’s office today, and chances are you’ll leave with a prescription. It’s not that your doctor isn’t well-intentioned. It’s that our healthcare system has been built to manage symptoms, not to address the root causes of illness.
Modern medicine is phenomenal at emergency intervention. It can save your life during a heart attack, remove a tumor, or stabilize a severe infection. But when it comes to the slow-burning issues, chronic fatigue, creeping weight gain, unexplained inflammation, brain fog, insulin resistance, or mood swings, the system often defaults to a quick fix. A pill for cholesterol. A sleep aid for insomnia. A statin for heart disease risk. One symptom, one solution.
This isn’t medicine—it’s maintenance.
But what if the real problem isn’t high cholesterol, but chronic inflammation fueled by poor diet, sedentary living, and unaddressed stress? What if mood swings aren’t a mental health disorder, but a hormonal imbalance driven by poor gut health or nutrient deficiencies? In many cases, the root cause is never fully explored. And so we block symptoms that we instead have to listen to because our body is trying to communicate something to us.
A System Designed to Manage Illness
Let’s be honest: there’s little financial incentive in prevention. The global pharmaceutical industry generates over $1.6 trillion annually, much of it from medications that manage, rather than cure, chronic conditions. Statins, insulin, antidepressants, and blood pressure medications generate billions each year. It’s a system that profits from keeping people alive, but dependent.
Meanwhile, the food industry pushes ultra-processed products loaded with sugar, seed oils, synthetic additives, and inflammatory chemicals, many of which have been linked to the very diseases medicine is trying to control. And these industries are deeply connected; pharmaceutical giants own stakes in food corporations, and vice versa. It’s a loop that keeps us sick, medicated, and constantly searching for “fixes” that never arrive.
The Cost of Ignoring Root Causes
We’re seeing the consequences. Chronic illnesses like Type 2 diabetes, heart disease, and even certain cancers are now being diagnosed in people in their 30s, 20s, and sometimes even younger. A recent study in Nature Reviews Clinical Oncology reported a sharp rise in early-onset cancer diagnoses globally, sparking concern across the medical community.
Why? Because we’re living in an environment designed for disease: fast food, screen time, stress, sedentary lifestyles, chemical exposures, sleep deprivation, and a constant state of sympathetic nervous system overdrive.
And our healthcare system isn’t designed to stop the train before it derails, it’s waiting with a bandage after the crash.
But what if we flipped that model?
What if we shifted our focus from disease care to health creation?
What if you could recognize early warning signs, before they turned into chronic conditions?
That’s where we’re headed next.
Recognizing the Warning Signs – Catching Disease Before Diagnosis
Most people don’t go from “healthy” to “sick” overnight. Disease is almost always a process, not an event. It builds slowly, and often silently, for years. But our current healthcare model waits until that process reaches a crisis point before doing anything about it.
By the time most people receive a diagnosis, whether it’s Type 2 diabetes, cardiovascular disease, or even cancer, they’ve likely been living in the early stages of dysfunction for a decade or more. Unfortunately, those early stages don’t always scream for attention. And if you don’t know how to listen, you miss the message.
The Body Always Speaks – Are you Listening?
So what are those early signals? They don’t always show up on routine lab tests, and they’re easy to dismiss as “just getting older” or “normal stress.” But they’re not.
- Persistent fatigue, even after a full night’s sleep
- Brain fog, difficulty concentrating, memory lapses
- Digestive issues like bloating, gas, or irregularity
- Weight gain or difficulty losing weight, especially around the belly
- Skin issues (acne, eczema, psoriasis)
- Mood swings, irritability, or low-level anxiety and depression
- Poor sleep quality, despite being exhausted
- Low libido or irregular menstrual cycles
These aren’t random annoyances. They’re red flags, early indicators of systemic imbalance, chronic inflammation, metabolic dysfunction, or hormonal disruption.
You don’t need a diagnosis to know your body is out of balance. You just need to start paying attention.
From Passive to Proactive
What if we normalized health check-ins before symptoms get serious?
There are critical health indicators you can start tracking today, to catch dysfunction early:
- Blood sugar regulation: Fasting glucose, HbA1c, and continuous glucose monitoring (CGM) can reveal insulin resistance before full-blown diabetes develops.
- Inflammation markers: C-reactive protein (CRP), homocysteine, and interleukin-6 levels offer insight into silent inflammation, which underpins nearly every chronic illness.
- Hormonal balance: Cortisol patterns, thyroid panels, and sex hormone levels (like estrogen, progesterone, testosterone) can expose imbalances early.
- Gut health indicators: Stool tests can reveal dysbiosis, leaky gut, or low microbial diversity—often long before symptoms escalate into IBS, autoimmune conditions, or even depression.
- Nutrient deficiencies: Common gaps in Vitamin D, magnesium, omega-3s, B12, and iron can affect energy, cognition, immunity, and mood.
The problem? Most routine checkups don’t include these markers. You’ll need to ask. You’ll need to advocate. You may even need to seek out more progressive or functional healthcare providers who understand how to catch problems in their earliest forms.
Learn to Speak the Language of Your Health
Think of this as health literacy 101. You don’t need to become a doctor, but you do need to understand the basics of your own biology. Because the earlier you detect imbalances, the easier they are to reverse.
As functional medicine pioneer Dr. Mark Hyman often says: “By the time you have a diagnosis, the horse has already left the barn.”
The good news? You don’t have to wait for a diagnosis. You can start today.
Up next, we’ll talk about how functional and personalized medicine is changing the way people stay healthy, not just treat illness.
The Shift to Preventive Medicine – Functional and Personalized Healthcare
If the traditional medical system is built to treat illness once it’s already taken root, then preventive medicine is about shifting the entire paradigm—catching dysfunction before it becomes disease, and personalizing care so it fits the individual, not the average.
That’s where functional and personalized medicine come in.
What Is Functional Medicine?
Functional medicine looks beyond symptoms and diagnoses. It asks: Why is this happening in the first place? What are the root causes, whether nutritional deficiencies, environmental exposures, lifestyle patterns, or genetic predispositions?
Unlike conventional medicine, which often treats one symptom with one drug, functional medicine recognizes that one root cause can trigger multiple symptoms, and that symptoms across the body may be connected.
A few key principles define this approach:
- Root cause analysis, not symptom suppression
- Biochemical individuality – no two bodies are alike
- The body as a complex, interconnected system
- Lifestyle as the foundation of healing
This model isn’t just theoretical, it’s now being embraced by thousands of clinics worldwide, including forward-thinking institutions like the Cleveland Clinic’s Center for Functional Medicine.
Personalization Is the Future of Healthcare
The era of one-size-fits-all healthcare is ending. Thanks to emerging science in genomics, metabolomics, and microbiome mapping, we can now tailor health strategies to each individual’s unique biology.
What works for one person may not work for another. Two people may have the same symptoms, but entirely different underlying causes.
That’s why personalization matters. From food choices and movement routines to supplementation and stress management, personalized protocols provide more effective outcomes than generic advice ever could.
And the tools to support that personalization are more accessible than ever.
Technology Is Making Prevention Easier (and Smarter)
What used to be expensive, lab-based, or only available through elite wellness clinics is now increasingly accessible to anyone with a smartphone or smartwatch.
- Wearables like Oura Ring, WHOOP, and Apple Watch track sleep quality, resting heart rate, heart rate variability (HRV), and activity levels. All data that can reveal early signs of stress, inflammation, or overtraining.
- Continuous Glucose Monitors (CGMs) provide real-time feedback on how your body responds to different foods, helping to fine-tune nutrition and prevent insulin resistance.
- At-home test kits for vitamin deficiencies, food sensitivities, microbiome diversity, and hormone levels make it easier than ever to monitor health from home.
- AI-driven health platforms are emerging that can analyze your health data and provide personalized recommendations, empowering users to take proactive steps long before symptoms set in.
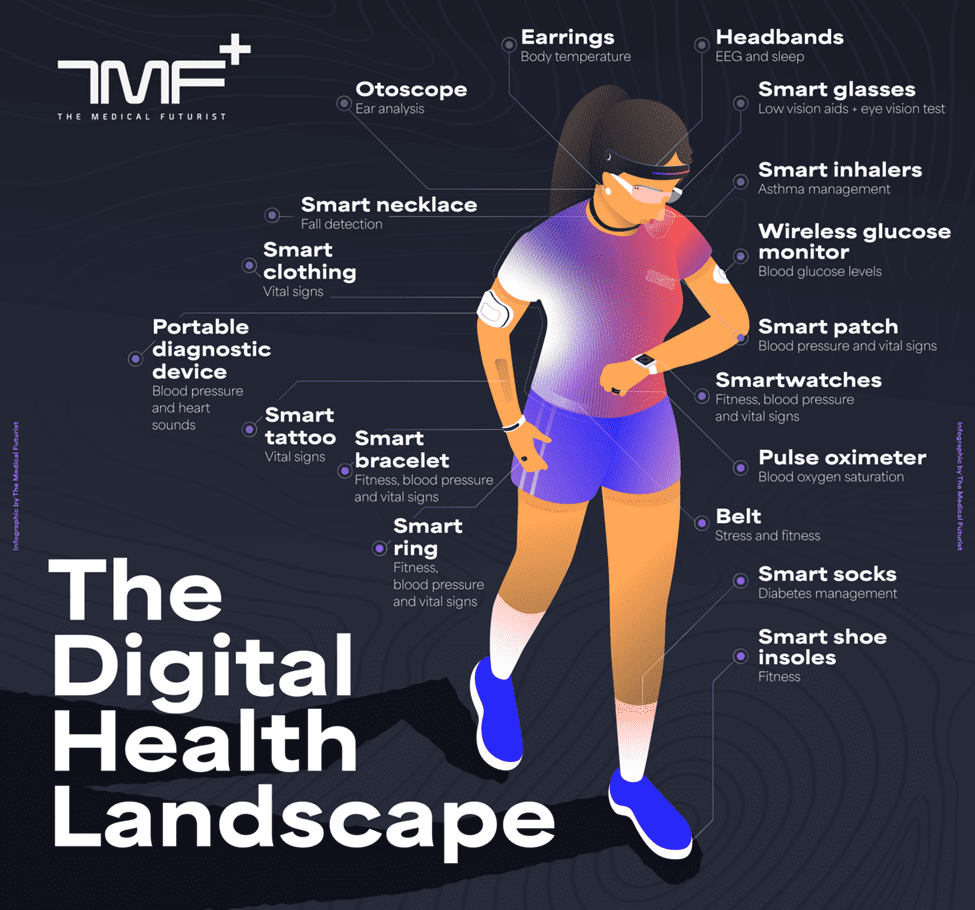
Source: The Medical Futurist
These tools aren’t meant to replace doctors, but they’re changing the role of the patient from passive recipient to active participant.
Why Early Intervention Saves Lives (and Costs Less)
The earlier you identify dysfunction, the easier it is to correct. That’s not just better for your long-term health, it’s also more affordable.
Treating early-stage insulin resistance through lifestyle changes is far cheaper, and more effective, than managing advanced diabetes with lifelong medication, insulin, and the complications that follow.
The same goes for heart disease, autoimmune conditions, hormone imbalances, and even some forms of cancer.
Put simply: Preventive care isn’t just good medicine, it’s good economics.
How to Take Control of Your Health: A Practical Guide
We’ve talked about what’s broken in the system and what needs to change—but what can you actually do today to protect your health before a diagnosis forces your hand?
Here’s a practical, no-nonsense guide to becoming the CEO of your own well-being. No medical degree required, just curiosity, commitment, and the willingness to take ownership of your body’s signals.
Step 1: Educate Yourself
Understanding your health is like learning a new language. And the best place to start is with voices that challenge convention and offer empowering, evidence-backed knowledge. These books belong on your shelf:
- “Outlive” by Dr. Peter Attia – A bold rethink of longevity that shifts the focus from lifespan to healthspan, with actionable strategies on nutrition, strength training, and disease prevention.
- “Good Energy” by Dr. Casey Means – A passionate call to tackle the root causes of chronic illness, showing how lifestyle and metabolic health shape everything from mood to immune function.
- “Glucose Revolution” by Jessie Inchauspé (The Glucose Goddess) – A compelling exploration of blood sugar regulation and its enormous impact on energy, cravings, and long-term disease risk.
- “Cancer as a Metabolic Disease” by Dr. Thomas Seyfried – A paradigm-shifting take on cancer biology that emphasizes mitochondrial dysfunction and nutrition-based therapies.
- “The Miracle Morning” by Hal Elrod – A practical blueprint for building a morning routine that supports clarity, vitality, and lasting well-being.
These resources aren’t fringe ideas, they’re the starting point for a different way of thinking about health: one that’s proactive, data-informed, and deeply personalized.
Step 2: Get Tested for Key Health Markers
All of this may sound great in theory—but where should you actually start? What tests or diagnostics can give you a clear picture of your health?
If you’re experiencing symptoms like fatigue, anxiety, low or high blood pressure, rapid heartbeat (tachycardia), daytime weakness, sleeping disorder, migraines, occasional constipation, or weight gain, don’t wait. And don’t settle for the standard “let’s observe” advice. Early action is key.
As Dr. Casey Means recommends in this Jay Shetty podcast, begin by checking a few simple health KPIs once or twice a year. If your markers fall within healthy ranges, your metabolic health is likely on track.
| Biological Marker | Description | Normal Range |
| Fasting Glucose | Measures blood sugar levels after fasting for 8+ hours. Indicator of insulin sensitivity and diabetes risk. | 70-99 mg/dL |
| Triglycerides | Type of fat in the blood. High levels increase heart disease and insulin resistance risk. | Less than 150 mg/dL |
| HDL Cholesterol | Known as ‘good’ cholesterol. Helps remove excess cholesterol; higher levels are protective. | Men: ≥40 mg/dL Women: ≥50 mg/dL Optimal: ≥60 mg/dL |
| Waist Circumference | Measures abdominal fat. High values linked to higher risk of metabolic and cardiovascular diseases. | Men: <40 in (102 cm), Women: <35 in (88 cm) |
| Blood Pressure | Measures force of blood against artery walls; key indicator of cardiovascular health. | Less than 120/80 mm Hg |
Most of these can be tested through standard labs or specialty wellness platforms like InsideTracker, Viome, or Genova Diagnostics.
If you notice any deviations, it’s time to take it seriously.
Find a reputable functional medicine doctor (by googling it) who can take a holistic view, investigate root causes, and guide you with personalized lifestyle changes, nutrition strategies, and supplements to help you restore balance and optimize your health.
Step 3: Use Technology to Your Advantage
You don’t need to live in a biohacking lab to benefit from technology. Here’s how to use everyday tools to stay ahead of the curve:
- Track Sleep & Recovery
- Devices like Oura Ring, Whoop, or Fitbit give you insights into how well your body recovers each night, a key factor in long-term health and immune resilience.
- Devices like Oura Ring, Whoop, or Fitbit give you insights into how well your body recovers each night, a key factor in long-term health and immune resilience.
- Monitor Blood Glucose in Real Time
- Continuous Glucose Monitors (CGMs) like Levels, Nutrisense, or Freestyle Libre can show you exactly how food, sleep, stress, and movement affect your metabolism.
- Continuous Glucose Monitors (CGMs) like Levels, Nutrisense, or Freestyle Libre can show you exactly how food, sleep, stress, and movement affect your metabolism.
- Heart Rate Variability (HRV)
- A key indicator of nervous system health. Higher HRV means better stress resilience, lower HRV signals the need for rest or stress management.
- A key indicator of nervous system health. Higher HRV means better stress resilience, lower HRV signals the need for rest or stress management.
- AI Health Dashboards
- Platforms like ZOE, InsideTracker, or MyVitalMetrics use AI to integrate your health data and recommend personalized interventions, what to eat, how to move, when to rest.
These tools aren’t about perfection—they’re about awareness. With just a few simple data points, you can course-correct before symptoms ever appear.
Step 4: Lifestyle First
You can’t out-supplement a bad diet. You can’t outsource your movement. You can’t biohack your way past stress.
Lifestyle is the foundation of health, and it always will be.
- Food as Medicine
- Prioritize whole, nutrient-dense foods. Eliminate ultra-processed products, refined sugar, industrial seed oils, and chemical additives.
- Focus on anti-inflammatory foods—leafy greens, omega-3 fats, fermented foods, and high-quality proteins.
- Consider time-restricted eating or intermittent fasting, under guidance, to support metabolic health.
- Move Daily
- You don’t need a gym. You need consistency.
- Walk more, lift heavy things, stretch, breathe. Movement is non-negotiable for blood flow, insulin regulation, and brain function.
- Stress, Sleep & Stillness
- Chronic stress is a silent killer. Prioritize mindfulness, breathing techniques, journaling, and social connection.
- Protect your sleep. No recovery = no resilience.
- Rest is not lazy, it’s necessary biology.
This is how we change the trajectory. One choice, one habit, one test at a time.
Why This Matters for Organizations and Employees
Let’s take a step back. You might be thinking, “This sounds great for individuals. But what does this have to do with organizations?”
The short answer? Everything.
We’re in an era where the health of your workforce is directly tied to the health of your business. Chronic illness, burnout, fatigue, anxiety, these aren’t just personal problems anymore. They’re performance problems, retention risks, and cost burdens that show up on your balance sheet whether you address them or not.
Chronic Illness Has Entered the Workplace
The same lifestyle-related diseases we’ve discussed, type 2 diabetes, cardiovascular conditions, autoimmune disorders, are increasingly showing up in the employee population, and often earlier in life. In fact, studies show that chronic health conditions account for 75% of healthcare costs for employers in the U.S.
What does this mean in practical terms?
- More sick days.
- More presenteeism (when employees show up but underperform).
- Higher insurance premiums.
- And increased turnover when burnout or illness becomes too much to manage.
This isn’t just about absenteeism, it’s about functional performance. An employee struggling with chronic fatigue or unmanaged stress can’t show up with clarity, creativity, or energy, no matter how skilled they are.
Health and Retention Are Now Linked
Let’s look at it from the employee’s point of view. After a global pandemic, workers are reevaluating what really matters, and health has shot to the top of the list. Millennials and Gen Z, in particular, are demanding more than a paycheck. They want workplaces that support their well-being, offer work-life balance, and prioritize mental health in actual policy.
If employers don’t adapt, employees will walk. And increasingly, they are.
A 2024 Deloitte study showed that nearly 40% of Millennials and Gen Z workers would leave a job that didn’t support their mental health. That’s not a fringe opinion, it’s a cultural shift.
Forward-Thinking Companies Are Taking the Lead
Some of the most admired companies today didn’t get there on product alone, they built people-first cultures where wellness is woven into the fabric of the business.
Take Salesforce, which offers comprehensive mental health days, wellness reimbursements, and internal employee resource groups that support well-being from multiple angles. Or Johnson & Johnson, whose workplace health strategy saved over $250 million in healthcare costs over a decade and delivered a $3 return on every $1 invested.
These companies understand something others are still catching up to: when your people thrive, so does your business.
A Shift from Perk to Responsibility
The biggest mistake companies make is treating wellness like a nice-to-have perk instead of a foundational business strategy.
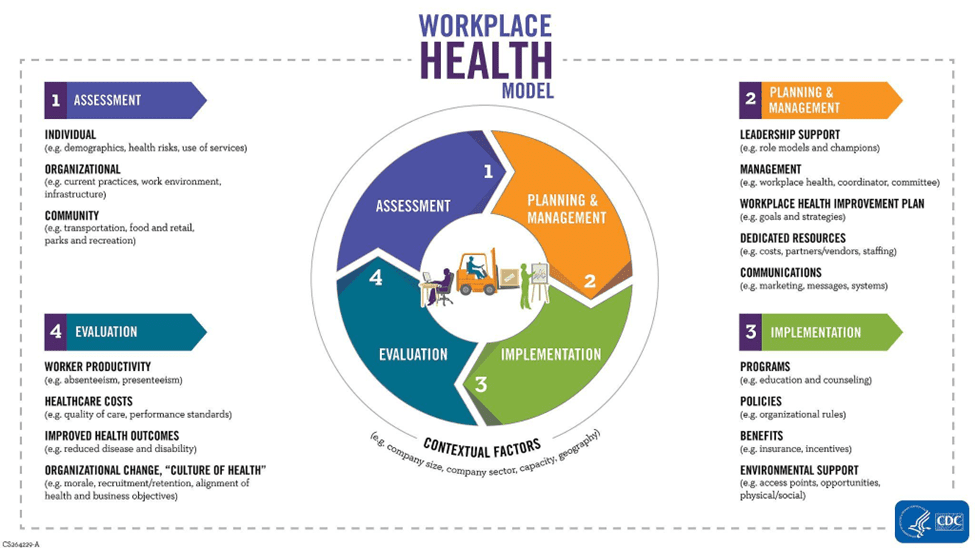
Source: CDC
The reality is this: companies now have a responsibility—not just ethically, but economically—to create environments that protect employee health before it deteriorates.
That means:
- Rethinking healthcare benefits beyond insurance plans
- Providing preventive screenings and lifestyle-focused health education
- Offering access to functional medicine approaches—not just reactive treatments
- Building wellness into culture, leadership training, and daily operations
And yes, this also means supporting employees in taking ownership of their own well-being. But they need the tools, permission, and space to do that—and leadership needs to model it.
Wellness is the Next Competitive Edge
Companies that invest in well-being today won’t just have healthier teams, they’ll have more loyal ones. More innovative ones. More resilient ones.
And in an age where burnout, chronic illness, and stress are draining organizations from the inside out, that’s not a luxury, it’s a survival strategy.
Conclusion: Your Health, Your Responsibility—But Also a Collective Opportunity
This article isn’t about fear, it’s about power. It’s a reminder that the most powerful changes often begin with awareness and small, consistent choices.
You don’t need to be a doctor to understand your own body. You don’t need to be wealthy to take proactive steps toward better health. And you don’t need a diagnosis to start treating your life like it matters.
Your health is your responsibility. Not because the system has failed, but because no system can care more about your future than you can.
But this isn’t just about individuals, either.
Leaders, managers, and HR professionals: this is your wake-up call, too. If you want to build high-performing teams, if you want to attract and retain the best people, if you want your organization to thrive in a chaotic, high-stress world, start by helping people stay well, not just helping them get better after they’ve burned out.
Because whether we’re talking about a person, a team, or an entire healthcare system—the real challenge isn’t just surviving longer.
It’s thriving longer.
Start now. Take stock of your health. Start asking better questions. Start making better choices. Start building cultures – at home, at work, in your communities – that make wellness the norm, not the exception.
And if you found this article helpful or thought-provoking, share it with someone who needs a reminder: there’s no such thing as “too early” or “too late” when it comes to protecting your health.
Subscribe to the Silicon Valley Innovation Center newsletter on LinkedIn for more expert insights on the biggest challenges and innovative solutions shaping today’s organizational landscape and personal wellbeing.